Clara Grimes, Deputy Director of Nursing, describes the impact of asking the WMTY? question with patients and staff.
Background to why we used WMTY approach
On reviewing the latest patient experience data in our Trust, the evidence showed there was an inconsistent approach to our communication with patients, including understanding what is important and valuable to them as individuals.
Our team agreed that Personalised Care is a key commitment for delivering health and high-quality care for all, as outlined in the NHS Long Term Plan (2019). We understand and see it is important to give patients the same choice and control over their mental and physical health that they expect in other aspects of their life, as this ensures better experiences and improved health and wellbeing.
A group of colleagues that included healthcare support staff, practice education staff, and clinical staff was formed and implemented the ‘A3 Thinking Project’. This was a problem solving, decision-making and collaborative plan to help coach and think through problem solving activities as well as communicate this learning to others. The aim of the A3 Thinking Project was to understand what could improve the fundamental care given to patients. We initially worked with two nominated wards.
The group’s action plan included the implementation of the WMTY? conversation tool across acute sites of the hospital.
How we used this approach
We implemented a test of change in two wards and developed a ‘buddying’ approach where the staff from both wards could support and drive each other to help implement the project. We gathered feedback from 72 patients across both wards from conversations between staff and patients. Patients told us that they were pleased to be asked about their wishes and preferences. We also reviewed the results of the inpatient postal survey which asked:
1. Do you feel listened to?
2. Do you feel that the staff had all the information that they needed in order to care for you?
3. Did you feel able to talk to members of hospital staff about your worries and fears?
4. To what extent did staff looking after you involve you in decisions about your care and treatment?
5. Did hospital staff keep you informed about what would happen next in your care and treatment during your stay?
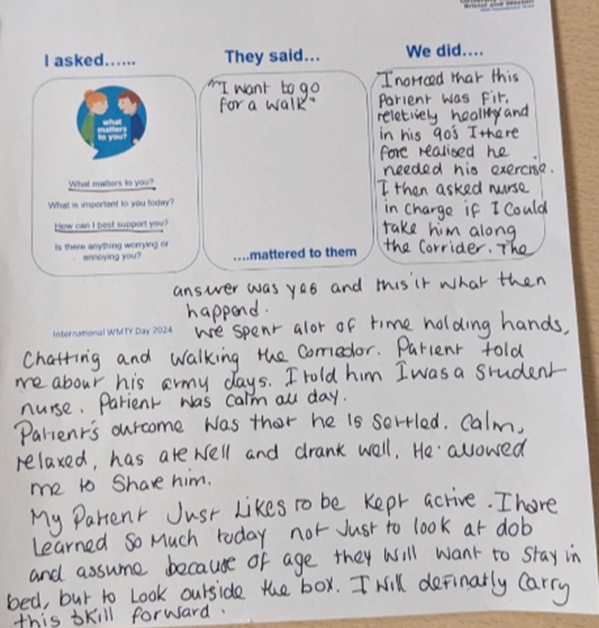
What was the outcome of the conversation?
52% of 25 staff who had WMTY? conversations with patients reported that they changed their care intervention because of asking the patient a ‘what matters’ question. This means that instead of the staff member doing what they would have intended to do, they spoke to the patient who required or wanted something different, so the care intervention was changed or altered for that patient.
Overall, 76% of the 25 staff said that they had shared what they had learnt about the patient with a relevant member of their multidisciplinary team. This is positive as it showed us that the conversations were being acted on and important information, pertinent to the individual was being shared amongst the team of professionals caring for the patient, and helping the staff to plan care with the patient’s wishes at the centre. Following this success, the WMTY? conversation was rolled out to all inpatient areas in accordance with the SMART action plan. WMTY? has been incorporated into the Trust’s Experience of Care Strategy 2024-2029, so it is a visible goal to all staff who work in the Trust. The project and strategy are bought to life by continually monitoring the impact and benefits to patients and celebrating and sharing successes and improvements.

What went well?
We planned activities around building relationships with patients and created opportunities for personalised conversations. Staff were able to explore patients’ individual characters, attributes and preferences to understand what is important to them.
On 6thJune, WMTY? day, we celebrated with lots of interactive activities. With the support of the arts team and volunteers, Divisions held lots of interactive activities for patients including, arts and crafts, singing, bowls, potting flowers, tea parties, quiz, nail painting and bingo.
We have embedded the WMTY? conversation approach into services across the Trust as well as incorporating the approach into the Experience of Care Strategy 2024-2029.
To help to share the work collaboratively with other health and social care providers, we have presented our work to the Heads of Patient Experience (HOPE) network which is an online meeting for peer learning and support for NHS leaders with responsibility for patient experience. This gave us the opportunity to meet national experts in patient experience research and improvement and learn from other innovations and best practice. We met with the leads of the NHS England Care Partner Initiative to discuss how they could use WMTY? Approach. Our Trust’s Experience of Care Strategy which incorporates WMTY? was also shortlisted for a prestigious Patient Experience Network National Award in October 2024.
Key challenges?
We understand that sustainable change takes time, support, and ongoing engagement to embed. We soon found that strong leadership was required to overcome resistance of staff, mainly around a preconceived idea that WMTY? created additional work for the healthcare staff.
Another key challenge was to involve staff as part of the strategy in formulating, planning and implementing the work. Engaging staff and colleagues was central to overcoming resistance to new ideas and different ways of working.
The project needed the time and focus of leaders to drive and embed the project; it was important to be visible and actively participate in WMTY? to motivate teams to do the same.
Key learnings?
WMTY? Staff focus
There were multiple ways in which we engaged teams in the roll out of WMTY? The first important engagement activity was a ‘What Matters to You?’ Staff Day. This was a day when staff were asked the question and responded via anonymous ‘blank space’ questionnaire where they had the freedom to express what was important to them.

As we were expecting staff to ask patients what is important to them, it felt just as important to understand what is important to staff. This helped staff to understand the purpose of WMTY? and its relevance. It was an opportunity to understand what was important to staff taking part and working towards their well-being.
These responses were collated and grouped into themes which were summarised into a ‘you said, we did’ poster to demonstrate where local leadership teams had listened to what was important to their team and made improvements as a result.
Improvement planning
We now want to embed the WMTY? conversation approach in all our services and healthcare pathways so that it becomes the way we open conversations with the people we support, empowering them to ask questions and make informed choices about their care and treatment options. We will continue to monitor the impact through our patient experience data as well as listening to anecdotal feedback from staff and patients.
The goal of asking patient WMTY? question has annual milestones over three years, and we recognise that cultural doesn’t change overnight.
Improving communication
We have learnt that patients and staff find the conversation tool beneficial in improving communication, so we do plan to continue to embed this initiative and change the culture to a communicative culture where patients are asked what is important to them, we listen and act where necessary.
The vision is that all people who use our services are actively engaged in conversations about what matters to them. Health consultations will bring together ‘the meeting of two experts’ where the patient (who is the expert in their life) makes choices and decisions with healthcare professionals, through asking ‘what matters to you?’